Antibiotic Pollution Index: 731 (19 November 2017)
What is the Antibiotic Pollution Index?
What it does
Chloramphenicol blocks the production of proteins in bacteria. When protein production is delayed, the bacterial cell stops to grow.
Who gets it
Chloramphenicol is a broad-spectrum antibiotic that is used to treat a large number of infectious diseases. Given a number of serious side effects, most physicians look for alternatives first before prescribing this drug, and in some countries it has been banned from the clinic. For instance, this drug has been linked to bone marrow damage, leading to anemia and potentially childhood leukemia. When risk groups are avoided or when the disease is life threatening, chloramphenicol is, however, an important drug: in regions with less sophisticated healthcare systems, it is used to treat meningitis, typhoid fever, plague and cholera.
The drug, although practically banned from medical use and meat production in many countries, is not reserved for people in need alone. It is still used for non-food producing animals around the world, and seafood production in Asia has become notorious for chloramphenicol pollution. Recently, this drug was seen in pharmacies that sell to fish and shrimp farms in Vietnam; and Chinese authorities found chemical traces in 9% of seafood found in restaurants in some major cities, including chloramphenicol.
Production and trade
It may be produced in India, Hungary, China, Japan, USA, Spain, Italy.
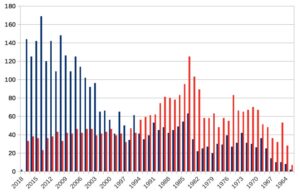
In 2016, Top-3 importers were Venezuela, Chile and the Netherlands; exporters were China, the Netherlands and India.
And, SquaredAnt, does it pollute?
18 Sites with environmental chloramphenicol residue in our database reside in Nigeria (waste water, river water and sludge) and Tianjin, China (agriculture soil). Especially in Nigeria, the concentrations are fairly high, up to ~100 ng/ml in sludge. Probably, this is due to a combination of medical and veterinary use, too: for instance, observations in 2012 showed that chloramphenicol has been routinely used in poultry farming in Nigeria.
The bacterium that produces chloramphenicol can be present in soil. Therefore it may be not as straightforward as it seems to distinguish polluting from naturally occurring trace amounts. A broad evaluation of historical land usage, irrigation sources and agricultural practices is crucial to rule out chemical pollution or its consequences (e.g. soil enrichment for chloramphenicol-producing bacteria).
Warning lights
Chloramphenicol was no popular drug, given a number of potentially serious toxic side effects. Whenever alternatives have become available, this drug has been phased out. In the recent years, it may have become more poplar, as a replacement for other antibiotics against which resistance has been developed. This is a warning light – not so much for chloramphenicol, but for the gravity of the overall AMR challenge. Increased usage of this antibiotic is probably an unsustainable solution in the longer term: chloramphenicol resistance genes have been detected on farms, and historical data shows that chloramphenicol resistance is common in places where it is used – and can extend to resistance against other antibiotics, too.
Any common sense in this antibiotic?
Chloramphenicol remains essential for treatment of life-threatening meningitis, typhoid fever, and other infections in developing countries. Chloramphenicol is slowly becoming a last resort drug, as a replacement for other, originally safer, and more effective antibiotics that are now phased out due to antibiotic resistance. The importance of this drug will therefore grow, therefore tighter restrictions on its usage in food production are needed.
Sources
- General information (wiki)
- Production, import and export
- Vietnamese aquaculture farmers’ drugs
- Chemicals in Chinese seafood
- Nigerian use of antibiotics in poultry
- Chloramphenicol in the soil
- Chloramphenicol resistance in wastewater from Swine feedlots
- Resistance in meningitis
- Come-back of chloramphenicol due to antibiotic resistance
- Come-back of chlormaphenicol due to antibiotic resistance(II)
- Co-resistance against chloramphenicol and other antibiotics