Antibiotic Pollution Index: 129 (19 November 2017)
What is the Antibiotic Pollution Index?
What it does
Nalidixic acid was discovered in 1962 and became the first antibiotic of the quinolone family. This family targets DNA synthesis in bacteria that leads to their death. Nalidixic acid mainly affects gram negative bacteria. Its successors, quinolones and fluoroquinolones drugs (such as norfloxacin), are less toxic and more effective against a broader spectrum of bacteria.
Who gets it
Nalidixic acid was commonly used to treat urinary tract infections, as it is rapidly secreted via the kidney and therefore reaches the urinary tract in a straightforward manner, both in humans as animals. These and other infections may be caused by food-borne pathogens such as Shigella, Salmonella and E. coli. Otherwise healthy individuals would be able to restore their own health, but dehydrated and/or undernourished children, elderly, and patients with a weak immune system, need medical treatment. In advanced healthcare systems, better alternatives are now available and this drug may be over its peak.
Where may it be produced?
Italy, India.
And, SquaredAnt, does it pollute?
We find minimal evidence for pollution of surface waters and waste effluents in Spain and in Australia. Concentrations tend to be low: the highest concentration is 0.06 ng/ml from a waste water treatment effluent in Spain. Or, from 17 billion liters of water you can harvest one dosage of 1 gram. The environmental concerns related to this drug, so far, seem to be limited.
Warning lights
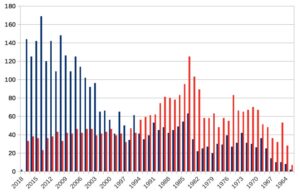
Many -but not all- types of resistance in the quinolone family include nalidixic acid resistance. As such, resistance against nalidixic acid may not be caused by nalidixic acid per se, and vice versa, resistance to other quinolone drugs may be caused by inadequate use of nalidixic acid. This is of importance when looking at resistance against this drug, which rose quickly after the turn of this century. In those years, in Germany, France, Spain, UK and Taiwan, an increase in the incidence of Salmonella strains that are resistant to nalidixic acid rose from ~5% to ~50% in humans and pigs. This occurred after the licensing of veterinary use of enrofloxacin and danloxacin, which belong to the same family as nalidixic acid. In 2004, resistance of Campylobacter bacteria against nalidixic acid in chicken and/or cattle throughout Europe reached 100%. An Australian study traced the origin of resistance against nalidixic acid in bacteria that cause enteric fever (Salmonella Typhi and Paratyphi). There, the share of resistant strains rose 70% in from 2009 to 2010. Most of these isolates came from India. Studies in the Shigella pathogens showed similar trends for Asian and African isolates. Summarized: nalidixic acid resistance itself is a warning light, very much a global phenomenon, and related to food production and food safety.
Any common sense in this antibiotic?
Nalidixic acid resistance is likely a result of the overuse of its family members. The sudden global rise in resistance has had a great impact on the interest from the academic community. Since 2000, resistance started to dominate the publications on nalidixic acid. In essence, nalidixic acid is a poster case for antibiotic resistance. In the past it was a popular drug, but now it mainly returns on resistance charts. Intriguing for scientists and a challenge for public health. If we learn from this pitfall, we may avoid others.
Sources
- production locations
- general information
- shigella resistance
- salmonella resistance+++
- salmonella resistance in pigs
- nalidixic acid resistance in food animals in Europe
- resistance in E. coil in poultry, Australia
- nalixic acid screening as marker for fluoroquinolone resistance
- mechanisms of resistance in fluoroquinolone family
- resistance of (fluoro)quinolones in food animals in Europe –> http://www.ema.europa.eu/docs/en_GB/document_library/Public_statement/2009/10/WC500005152.pdf